It might surprise you to learn that what you choose for your massage therapy business name can make a big difference in how well your massage business does. Consider your name a marketing tool.
Why? Your name can convey a lot of information, or it can convey no information, or it can convey the wrong information. In all cases, it makes a statement about your business, often the first impression a new client gets about you. A business name is not just a name, it is a description. Your name automatically tells a marketing story.
What kind of information can a potential and existing client get from your massage therapy business name?
Business service type – if your name does not indicate that you provide massage services, then a potential client has to find that out elsewhere.
Style of work – your name might be able to let them know if you are more focused on medical/treatment work, or more relaxation/spa work, or another style.
Wealth factor – if your business caters to the very wealthy, or instead you want to provide massage for people who normally can't afford it, your name could help let people know what they can expect.
Location – if your location is very favorable, having the location in the name might be very good. (But to do this you have to be pretty sure you will be in your location for a significant length of time.)
In fact if you have any very unique focuses for your business, that really make you stand out from other business in your area, this might be some information that you could convey in your massage therapy business name. Don't do this lightly though. You have to be very sure about your business direction and U.S.P. to have your name focused on it. But if you are sure, go for it. It could make a big difference.
Try not to choose your massage therapy business name just because you like it (and don't feel bad if you did, I have many times). It is far easier and better for your business if you choose a name that helps solve some problems of your target market. It is even better if you also like it!
Carefully consider each step your potential clients have to go through to find you. As they look in the yellow pages, if your name contained valuable insights that would help them narrow their search down to you, that would really help them. When your current clients describe you and your business name to friends, it might really help if your business name helped make clear what it is about you that is unique.
For some, having a business name that really helps support their U.S.P. may be easy. But for most therapists starting their businesses it will be more of a learning curve. Developing a good U.S.P. is not that easy and generally takes some experience within your business.
And the fact is you it is hard to create a good business name in either case unless you have a pretty clear business plan. You need to be very clear about what your main focus of your business is before you choose your business name.
Most folks start with a massage therapy business name, and then work on what their business is going to be. I really encourage you to develop your business plan as far as you can first, and then choose a business name that supports your unique business direction.
When choosing a name be careful about getting stuck in a too small a box.
Here are a couple of more points to consider before finalizing your massage therapy business name:
Pick a name that allows your business to grow. Don't narrow yourself down too much. Imagine where you want your business to be five years down the road and make sure your name will support these goals.
Consider a name that still has a web domain available, with a .com ending.
Make it easy to hear, say, and spell. If someone told a friend your business name, would they be able to understand it easily and spell it? Would it sound too much like something else and be confusing? Does it need explaining? Does it roll easy off the tongue, and sound good? Does it work well in print?
Maybe make it unique. Why have a name for your business that is only a little different than everyone else?
Think about how your business name positions you in relation to your local competition. When your ads are seen together, what will your target market be thinking?
What story does your massage therapy business name tell? Is it what you want your clients to hear?
Make sure someone does not already have a trademark on your chosen business name. You can use the free Search It! tool to do a domain name check, and also under the category Site Legalities you can select Trademark check.
And before you finalize it, check in with friends, family and business mentors to make sure you have not missed anything. But also keep your focus in mind. Most of your friends and family are not trained in marketing.
The #1 piece of advice though is to have a clear business plan developed before you choose your name. Your name is a marketing tool that you will likely use for the length of your business. So put a lot of effort into planning your business first!
And if you already have a massage therapy business name you are not happy with you can consider changing it. It really depends on how many people already identify with your current name, and how long you have been using it. I would say if you have not been in business for too long, and you think changing your name could make a dramatic improvement in helping grow your business, it might be worth the effort. If you do change it, make sure you don't abandon the old one completely. For at least a year have a statement under your new name that reads: previously – (your old name here).
Finally, when you are brainstorming new massage therapy business name options, write down as many as you can possibly think about. Then carefully evaluate each one, and weed it down to the best three. Then show these to your friends and family.
OK, have fun!
Sarcomere
A sarcomere is the basic unit of a muscle's cross-striated myofibril. Sarcomeres are multi-protein complexes composed of three different filament systems.
The thick filament system is composed of Myosin protein which is connected from the M-line to the Z-disc by titin. It also contains myosin-binding protein C which binds at one end to the thick filament and the other to Actin.
The thin filaments are assembled by Actin monomers bound to nebulin, which also involves tropomyosin (a dimer which coils itself around the F-actin core of the thin filament) and troponin.
Nebulin and titin give stability and structure to the sarcomere.
A muscle cell from a biceps may contain 100,000 sarcomeres. The myofibrils of smooth muscle cells are not arranged into sarcomeres.

Golgi Tendon Organ
Muscle Spindle

Muscle spindles are sensory receptors within the belly of a muscle, which primarily detect changes in the length of this muscle. They convey length information to the central nervous system via sensory neurons. This information can be processed by the brain to determine the position of body parts. The responses of muscle spindles to changes in length also play an important role in regulating the contraction of muscles, by activating motoneurons via the stretch reflex to resist muscle stretch.
Extrafusal muscle fibers are innervated by alpha motor neurons(highly myelinated) and generate tension by contracting, thereby allowing for skeletal movement.
Intrafusal muscle fibers are innervated by gamma motor neurons(less myelinated) and thus serve as a sensory proprioceptor.
The static axons innervate the chain or bag2(largest) fibers. They increase the firing rate of Ia(primary) and II(secondary) afferents at a given muscle length (see schematic of fusimotor action below).
The dynamic axons innervate the bag1(smaller) intrafusal muscle fibers. They increase the stretch-sensitivity of the Ia(primary) afferents by stiffening the bag1 intrafusal fibers.
The alpha motor neuron and the extrafusal muscle fibers it innervates make up the motor unit. The connection between the alpha motor neuron and the extrafusal muscle fiber is a neuromuscular junction, where the neuron's signal, the action potential, is transduced to the muscle fiber by the neurotransmitter acetylcholine.
http://www.angeltear.com/spindle/spindle.html
Angle of Torsion
Torsions of the osseous structure of the lower extremity affect not only the angle of gait but also the function of the foot. The principle torsions of clinical interest are femoral torsion and malleolar torsion. The clinical picture of femoral torsion is complicated by positional (soft tissue) relationships of the hip. This treatise will describe the normal torsional relationship of the hip first, followed by the positional relationships of the femur to the pelvis, then the abnormal torsional relationships of the femur, and finally the torsion of the tibia. The effects on foot function and gait will be described at the end of the treatise.














NORMAL TORSION OF THE FEMUR:
In the normal adult, the head and neck of the femur are angulated by 12 degrees relative to the femoral condyles as noted in the illustration below.

POSITIONAL RELATIONSHIP OF HIP ("VERSION" ANGLES)
In the normal adult the Head and Neck of the Femur is angulated approximately 12 degrees relative to the frontal plane of the body. In other words, the angle of the head and neck of the femur is measure relative to the posterior pelvis. Note that the leg faces straight forward. The gluteal fold is drawn for purposes of orientation only and is obviously not anatomically accurate. This represents a normal femur correctly "positioned" into the acetabulum. Note that the angle that the head and neck of the femur makes with the femoral condyles is identical to the angle that the head and neck make with the frontal plane of the body.

ANTEVERSION is an increase in the angle of the head and neck of the femur relative to the frontal plane of the body. This represents a normal femur abnormally positioned in the acetabulum. The net effect of this positional relationship is an externally rotated leg.

RETROVERSION is a decrease in the angle of the head and neck of the femur relative to the frontal plane of the body. This represents a normal femur that is abnormally positioned relative to the acetabulum. The net effect of this positional relationship is an internally rotated leg.

In the three preceeding illustrations the angular relationship between the head and neck of the femur and the femoral condyles (torsion) is normal. These three illustrations describe the positions of a normal femur relative to the frontal plane of the pelvis.
In the following description of femoral torsional abnormalities, it is important to understand that the angle that the head and neck of the femur make with the frontal plane of the body is 12 degrees. In other words the position of the head and neck relative to the pelvis is normal but the torsion within the bone is abnormal.
ANTETORSION is an increase in the angle of the head and neck of the femur relative to the femoral condyles as noted below. An angle of 30 degrees is shown. Note that the angle that the head and neck of the femur make with the frontal plane of the body is normal and therefore Antetorsion results in an internally deviated thigh.

RETROTORSION is a decrease in the angle of the head and neck of the femur relative to the femoral condyles. In the illustration the angle is approximately 8 degrees. Note that the angle that the head and neck of the femur make with the frontal plane of the body is normal and therefore Retrotorsion results in an externally deviated thigh.

For purposes of clarity, the following illustrates the superimposition of normal torsion, retrotorsion, and antetorsion.

Remember: when speaking of the TORSION angles, the head and neck of the femur are measured relative to the condyles of the femur. When speaking of the VERSION angles, the head and neck are measured relative to the frontal plane of the body.
To keep the terminology and concepts without confusion, I suggest the following crutch. If Antetorsion causes and internal rotation of the limb then Retrotorsion will cause an external rotation of the limb. If Antetorson causes an internal deviation and Anteversion will cause the opposite i.e., external rotation.
In the normal adult, the "Torsion" angle equals the "Version" angle. "Torsion"="Version"=12 degrees.

At birth, the torsion within the femur and the position of the femur relative to the frontal plane of the body are markedly different from adult values. Examination of the newborn should demonstrate an externally rotated limb by approximately 30 degrees.
Antetorsion=30 degrees
Anteversion= 60 degrees
Anteversion= 60 degrees

The limb is externally rotated because the increase in anteversion is 30 degrees greater than the increase in antetorsion.
From birth to adulthood anteversion decreases from 60 degrees to 12 degrees for a difference of 48 degrees. Therefore the net effect of this decrease is a positional change of 48 degrees resulting in a less externally deviated limb. At the same time, Antetorsion reduces from 30 degrees to 12 degrees for a difference of 18 degrees. The net effect of this decrease in antetorsion is a structural change resulting is less internal deviation of the limb. These changes usually occur in the first six years of life but may be delayed until adolescence.

Statistically, 95% of abnormal torsion of the femur reduces by adolescence. Between age 6 and adolescence, the presence of an in-toe gait secondary to an internal torsion may indicate a torsional abnormality that may proceed into adulthood or a delay in development. While the clinician may have to wait for adolescence to verify spontaneous reduction, a good clue may be found in the families of the child's parents. The presence of an in-toe gait within the child's adult family is highly suggestive of a true torsional abnormality (and the limb will not derotate with time) while the absence of an adult with an in-toe gait within the child's family indicates delayed development and probable spontaneous resolution.
At birth there is no tibial (malleolar) torsion but soon develops with weight bearing. Normal adult value for malleolar torsion is 18 to 23 degrees. A decrease in this value leads to an adducted gait while and increase in this value leads to an abducted gait. The position of the foot in the transverse plane (abducted or adducted) is not readily altered by gait plates (see later).

THE CLINICAL PICTURE
The following description of the clinical presentation is divided into two parts. The first describes the most common responses for the foot i.e., downward compensations while the latter will describe the uncommon but intriguing upward compensations that are associated with internal torsions of the femur.
With either a retrotorsion or an anteversion, the limb will be externally deviated and the neutral position of the hip rotations will be external. The knee and foot will function externally and an increase in the angle of gait will be noted clinically. With external torsions/positions there is a retrograde pronatory force on the foot that can be easily demonstrated. If you stand up, abduct your feet significantly, and lean forward and (voila!) your feet will pronate, illustrating the retrograde pronatory force. Abducted gait secondary to external torsion/position of the femur respond well to foot orthoses. A standard device will usually reduce the angle of gait to normal limits but on occasion a gait plate may be necessary.
With either an antetorsion or a retroversion, the limb will function internally deviated and the neutral postions of the range of motion of the hip will be internal. In gait, the knee is readily noted to be internally deviated. At this point the patient has three choices: (a) let the limb and foot be internally deviated (adducted foot), (b) use active muscle contraction to externally rotate the hip or (c) contract peroneus brevis muscle to abduct the foot.
In the uncomplicated scenario the foot will be adducted and the foot will have a retrograde supinatory force. (Stand up, adduct your feet and lean forward and (voila!) the foot supinates.) The problem with an adducted gait is primarily cosmesis, not function; the foot does well, all things considered.
The pigeon toe gait is usually unacceptable to adults and children and compensations result. With children, either the parents or the child realize the gait is peculiar and attempt to alter the angle of gait. The limb could be rotated externally at the hip but this takes too much muscle effort. It is much easier and more efficient to contract the peroneus brevis muscle to abduct the foot and thereby produce a more normal angle of gait. The peroneus brevis is normally a stance phase muscle that is recruited to fire during the swing phase of gait to abduct the foot. Unfortunately, the foot is abducted (pronated) in swing, abducted and pronated during the entire stance phase of gait from heel contact through toe off. This is open kinetic chain pronation of the foot. The foot never resupinates and is generally a very pathological , symptomatic and subluxed foot. Shoe wear is pathonomonic: excessive wear on the medial aspect of the heel and the medial aspect of the sole of the forefoot and the footgear is generally short lived.
Thus with internal deviations, two extremes may be seen: a child/adult with an adducted gait with a retrograde supinatory force on the foot or a relatively normal angle of gait with a subluxed foot secondary to open kinetic chain contraction of the peroneus brevis muscle.
When using orthotics to treat a flat foot secondary to an internal deviation of the limb cosmesis is once again a concern. Control of the pronated foot with regular orthotics will lead to an adducted gait. Both adults and children should be informed of this consequence. Gait Plates may be employed but the response is not uniform. It is generally true that Gait Plates positively alter the angle of gait for torsional and positional abnormalities of the femur but usually do not alter the angle of gait for torsional abnormalities of the tibia (increased or decreased malleolar torsion).
Upward compensation for internal torsions are intriguing. As mentioned earlier, downward compensation for an internal femoral torsion (antetorsion) the extremes of foot function may be represented by an adducted gait (with relatively good foot function) or a very flat foot (open kinetic chain pronation) with a relatively normal angle of gait. Upward compensations are usually associated with a unilateral internal torsions or assymmetrical bilateral internal torsions, i.e., one extremity is more severely affected than the opposite extremity.
Illustrated below are unilateral internal torsions of the femur on the right extremity. The first illustration shows a pelvis, its plane of progression (straight ahead), a normal left extremity and an internally deviated right extremity. The right foot may be adducted or it may be subluxed secondary to open kinetic chain pronation. In the second illustration (same scenario of internal torsion of the right limb only) the patient has learned to lead with the opposite hip (upward compensation). Although the pelvis is oblique, the plane of progression of the body remains straight ahead. Note that the right limb is parallel to the plane of progression thereby decreasing the necessity for right pedal compensation, although it may still occur but to a lesser extent. Most interesting in the end result to the left extremity. Now the left limb is internal relative to the plane of progression but is in normal alignment relative to the pelvis. Note that the foot which is opposite to the side of the deformity is internally deviated (adducted) relative to the plane of progression.


Clinically, the left foot may be adducted and relatively stable. The other extreme is that the left foot could be subluxed secondary to open kinetic chain pronation (attempting to improve the angle of gait). In this last example the flat foot is on the opposite limb to the major deformity.
Hip leading (upward compensation) will also occur with bilateral but asymmetrical internal torsions, or in other words one limb is more severely affected with internal torsion. In these cases the hip leading is always on the opposite side to the major deformity.
Hip leading is readily observable in gait. At heel contact, the affected side always displaces further forward than the opposite pelvis at heel contact. The obliquity of the pelvis relative to the plane of progression can be observed when looking at a complete gait cycle. Remember, the pelvis is still oscillating in the transverse plane but functioning obliquely to the plane of progression.
Q Angle

The quadriceps angle (Q angle) is determined by drawing one line from the anterior superior iliac spine through the center of the patella and a second line from the center of the patella through the tibial tuberosity. A Q angle greater than 15 degrees is a predisposing factor for patellar subluxation (i.e., if the Q angle is increased, forceful contraction of the quadriceps muscle can cause the patella to sublux laterally).
Foot

tarsus (7 tarsal bones) talus, calcaneus(calcaneus tuberosity), navicular, cuboid, lateral cuneiform, intermedial cuneiform, medial cuneiform
metatarsus (5 metatarsal bones)
toes (14 phalanges)
hallux - big toe - proximal, distal
2nd - 5th phalanges - proximal, meddle, distal
medial plantar arch
Coxa Vara & Coxa Varus

Coxa valga is a deformity of the hip where the angle formed between the head and neck of the femur and its shaft is increased, usually above 135 degrees. It is caused by a slipped epiphysis of the femoral head
Coxa vara is a deformity of the hip, whereby the angle between the ball and the shaft of the femur is reduced to less than 120 degrees. This results in the leg being shortened, and therefore a limp occurs. It is commonly caused by injury, such as a fracture. It can also occur when the bone tissue in the neck of the femur is softer than normal, meaning it bends under the weight of the body. This may either be congenital, also known as Mau-Nilsonne Syndrome, or the result of a bone disorder. The most common cause of coxa vara is either congenital or developmental. Other common causes include metabolic bone diseases (e.g. Paget's disease of bone), post Perthes deformity, osteomyelitis, and post traumatic (due to improper healing of a fracture between the greater and lesser trochanter). Shepherds Crook deformity is a severe form of coxa vara where the proximal femur is severely deformed with a reduction in the neck shaft angle beyond 90 degrees. It is most commonly a sequellae of osteogenesis imperfecta, Pagets disease, osteomyelitis, tumour and tumour-like conditions (e.g. fibrous dysplasia).
Pelvis
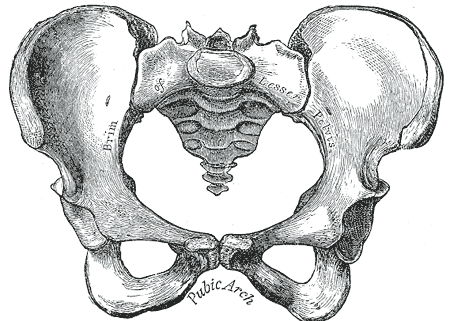
female pelvis
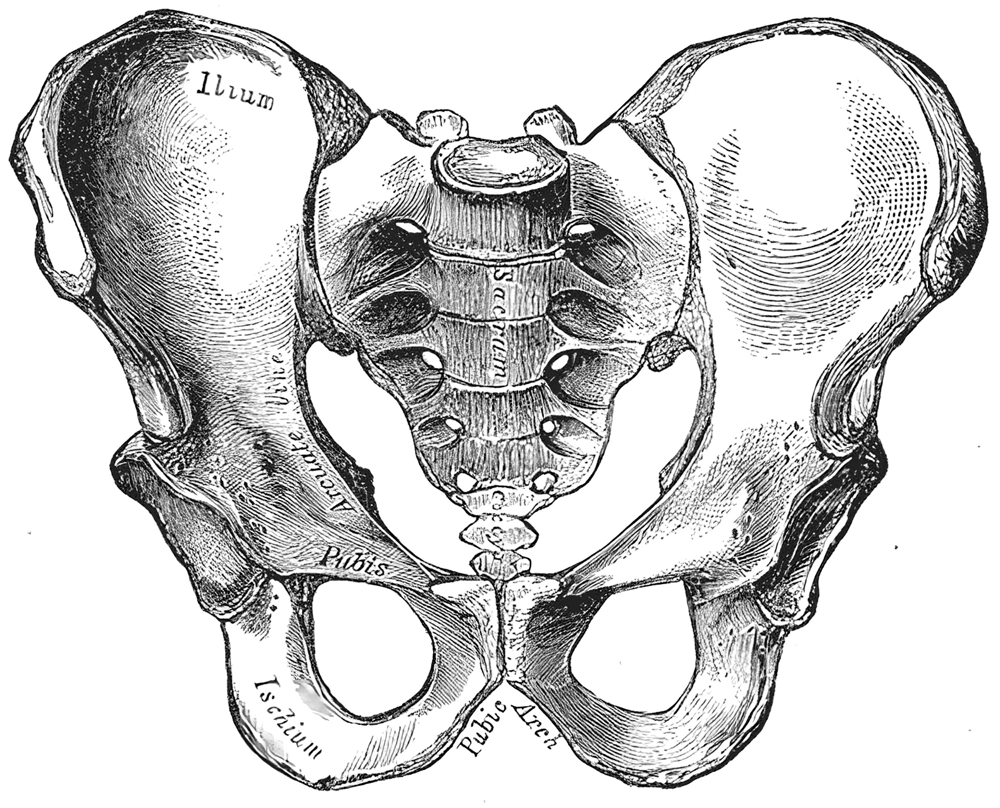
male pelvis


Ilium
ala(wing) of ilium (gluteal surface)
iliac crest
intermediate zone, tuberculum, outer lip, inner lip
gluteal lines
anterior, inferior, posterior
psis - posterior superior iliac spine
asis - anterior superior iliac spine
piis - posterior inferior iliac spine
aiis - anterior inferior iliac spine
greater sciatic notch
ischial spine
iliac tuberosity/tubercle
arcuate line
auricular surface (for sacrum)
Ischium
ischial spine
ischial tuberosity
lesser scitic notch
acetabulum
inferior ramus of pubis
ramus of ischium
Pubis
lunate surface
inferior pubic ramus
margin/limbus of acetabulum
obturator foramen
superior pubic ramus
pubic tubercle
obturator crest
Hallux Valgus & Hallus Varas
The term "hallux valgus" or "hallux abducto-valgus" are the most commonly-used medical terms associated with a bunion anomoly, where "hallux" refers to the great toe, "valgus" refers to the abnormal angulation of the great toe commonly associated with bunion anomolies, and "abductus/-o" refers to the abnormal drifting or inward leaning of the great toe towards the second toe, which is also commonly associated with bunions.

Hallus Varas is a deformity of the great toe joint where the hallux is deviated medially (towards the midline of the body) away from the first metatarsal bone. The hallux usually moves in the transverse plane.


Hallus Varas is a deformity of the great toe joint where the hallux is deviated medially (towards the midline of the body) away from the first metatarsal bone. The hallux usually moves in the transverse plane.

Cartilage Tissue
Note: This page is part of the section about the structure and function of different Tissue Types, which is related to the section about Histology and Cells (incl. structure of animal cells, cell division, mitosis, meiosis). This "Tissue Types" section is included to complete description of the knowledge of "Histology - The Cell" required by some courses in First-Level Anatomy and Physiology. To read about other tissue types see the list of on the left.
In the fetus and infant cartilage occurs in many parts of the body but much of this juvenile cartilage disappears during growth and development. The information on this page is concerned primarily with cartilage tissue in adult humans.
The Structure (Physical Description) of cartilage tissue in general
Cartilage is a connective tissue consisting of a dense matrix of collagen fibres and elastic fibres embedded in a rubbery ground substance. The matrix is produced by cells called chondroblasts, which become embedded in the matrix as chondrocytes.
That is, mature cartilage cells are called chondrocytes.
They occur, either singly or in groups, within spaces called lacunae (sing. lacuna) in the matrix.
The surface of most of the cartilage in the body is surrounded by a membrane of dense irregular connective tissue called perichondrium. This is important to remember especially because (unlike other connective tissues), cartilage contains no blood vessels or nerves - except in the perichondrium.
There are three different types (structures) of cartilage that have slightly different structures and functions.
They are hyaline cartilage, fibrocartilage, and elastic cartilage, described seperately in the sections below:
Hyaline Cartilage
1.0 Where in the body is hyaline cartilage tissue ?
Hyaline cartilage is the most abundant of the three types of cartilage.
It is found in many locations in the body, including:
Bronchi; Bronchial Tubes; Costal Cartilages; Larynx (voice-box); Nose; Trachea
Covering the surface of bones at joints - especially in areas where damage due to wear may lead to osteoarthritis incl. e.g. the ends of the long bones, and also the anterior ends of the ribs.
Embryonic skeleton (i.e. in the fetus).
2.0 The Structure of hyaline cartilage tissue
Hyaline cartilage consists of a bluish-white, shiny ground elastic material with a matrix of chondroitin sulphate into which many fine collagen fibrils are embedded. It contains numerous chondrocytes.
See the diagrams of the structure of cartilage tissue.
3.0 The Functions of hyaline cartilage tissue
Hyaline cartilage tissue provides smooth surfaces, enabling tissues to move/slide easily over each other, e.g. facilitating smooth movements at joints. It is also provides flexibility and support.
Fibrocartilage
1.0 Where in the body is fibrocartilage tissue ?
Examples include:
Calli (sing. callus), which is the tissue formed between the ends of the bone at the site of a healing fracture (bloodclot -> granulation tissue -> cartilage -> bone);
Intevertebral discs (i.e. the discs between the vertebrae of the spine);
Menisci (cartilage pads) of the knee joint.
Pubic symphysis, which is the position at which the hip bones join at the front of the body.
Also in the portions of the tendons that insert into the cartilage tissue, especially at joints.
2.0 The Structure of fibrocartilage tissue
Fibrocartilage is a tough form of cartilage that consists of chondrocytes scattered among clearly visible dense bundles of collagen fibres within the matrix. Fibrocartilage lacks a perichondrium.
See the diagrams of the structure of cartilage tissue.
3.0 The Functions of fibrocartilage tissue
Fibrocartilage tissue provides support and rigidity to attached/surrounding structures and is the strongest of the three types of cartilage.
Elastic Cartilage
1.0 Where in the body is elastic cartilage tissue ?
Auditory (Eustachian) Tubes;
External Ear (Auricle);
Epiglottis (the lid on the top of the larynx).
2.0 The Structure of elastic cartilage tissue
In elastic cartilage, which is yellowish in colour, the cartilage cells (chondrocytes) are located in a threadlike network of elastic fibres within the matrix of the cartilage. A perichondrium is present.
See the diagrams of the structure of cartilage tissue.
3.0 The Functions of elastic cartilage tissue
Elastic cartilages provides support to surrounding structures and helps the define and maintain the shape of the area in which it is present, e.g. the external ear.
In the fetus and infant cartilage occurs in many parts of the body but much of this juvenile cartilage disappears during growth and development. The information on this page is concerned primarily with cartilage tissue in adult humans.
The Structure (Physical Description) of cartilage tissue in general
Cartilage is a connective tissue consisting of a dense matrix of collagen fibres and elastic fibres embedded in a rubbery ground substance. The matrix is produced by cells called chondroblasts, which become embedded in the matrix as chondrocytes.
That is, mature cartilage cells are called chondrocytes.
They occur, either singly or in groups, within spaces called lacunae (sing. lacuna) in the matrix.
The surface of most of the cartilage in the body is surrounded by a membrane of dense irregular connective tissue called perichondrium. This is important to remember especially because (unlike other connective tissues), cartilage contains no blood vessels or nerves - except in the perichondrium.
There are three different types (structures) of cartilage that have slightly different structures and functions.
They are hyaline cartilage, fibrocartilage, and elastic cartilage, described seperately in the sections below:
Hyaline Cartilage
1.0 Where in the body is hyaline cartilage tissue ?
Hyaline cartilage is the most abundant of the three types of cartilage.
It is found in many locations in the body, including:
Bronchi; Bronchial Tubes; Costal Cartilages; Larynx (voice-box); Nose; Trachea
Covering the surface of bones at joints - especially in areas where damage due to wear may lead to osteoarthritis incl. e.g. the ends of the long bones, and also the anterior ends of the ribs.
Embryonic skeleton (i.e. in the fetus).
2.0 The Structure of hyaline cartilage tissue
Hyaline cartilage consists of a bluish-white, shiny ground elastic material with a matrix of chondroitin sulphate into which many fine collagen fibrils are embedded. It contains numerous chondrocytes.
See the diagrams of the structure of cartilage tissue.
3.0 The Functions of hyaline cartilage tissue
Hyaline cartilage tissue provides smooth surfaces, enabling tissues to move/slide easily over each other, e.g. facilitating smooth movements at joints. It is also provides flexibility and support.
Fibrocartilage
1.0 Where in the body is fibrocartilage tissue ?
Examples include:
Calli (sing. callus), which is the tissue formed between the ends of the bone at the site of a healing fracture (bloodclot -> granulation tissue -> cartilage -> bone);
Intevertebral discs (i.e. the discs between the vertebrae of the spine);
Menisci (cartilage pads) of the knee joint.
Pubic symphysis, which is the position at which the hip bones join at the front of the body.
Also in the portions of the tendons that insert into the cartilage tissue, especially at joints.
2.0 The Structure of fibrocartilage tissue
Fibrocartilage is a tough form of cartilage that consists of chondrocytes scattered among clearly visible dense bundles of collagen fibres within the matrix. Fibrocartilage lacks a perichondrium.
See the diagrams of the structure of cartilage tissue.
3.0 The Functions of fibrocartilage tissue
Fibrocartilage tissue provides support and rigidity to attached/surrounding structures and is the strongest of the three types of cartilage.
Elastic Cartilage
1.0 Where in the body is elastic cartilage tissue ?
Auditory (Eustachian) Tubes;
External Ear (Auricle);
Epiglottis (the lid on the top of the larynx).
2.0 The Structure of elastic cartilage tissue
In elastic cartilage, which is yellowish in colour, the cartilage cells (chondrocytes) are located in a threadlike network of elastic fibres within the matrix of the cartilage. A perichondrium is present.
See the diagrams of the structure of cartilage tissue.
3.0 The Functions of elastic cartilage tissue
Elastic cartilages provides support to surrounding structures and helps the define and maintain the shape of the area in which it is present, e.g. the external ear.
Subscribe to:
Posts (Atom)
